Capacity Without Clarity: Rethinking Patient Access Bottlenecks
Still facing access issues despite new tools? Here’s what most systems overlook—and how to fix it.
As workforce shortages, rising costs, and evolving consumer expectations converge, health system leaders are renewing their focus on a longstanding issue: patient access. Despite investing in centralized contact centers, EMR upgrades, AI-enabled scheduling tools, and digital front doors, many health systems struggle with timely availability, appointment scheduling, and efficient provider time management.
Patient Access Delays Are Worsening
According to a recent AMN Healthcare survey, average wait times for new patient appointments have reached a record high of 31.5 days, a 19% increase since 2022. For OB-GYN and cardiology, waits stretch to 42 and 33 days, respectively. Meanwhile, the AAMC projects a national shortfall of up to 86,000 physicians by 2036, compounding the supply-demand mismatch.
Executives are taking notice. More than half (52%) of health system leaders in a Vizient study identified patient access, throughput, and capacity as their top priority for 2025—outranking financial margin and digital transformation. At the provider level, 71% of respondents to Experian Health’s 2025 State of Patient Access Survey said appointment scheduling and availability was their most significant challenge.
Despite years of effort and investment, many health systems still struggle to deliver timely access, user-friendly scheduling, and optimized provider utilization. The result? Frustrated patients, overwhelmed providers, and leaders with limited insight into root causes.
Why the Disconnect?
This isn’t a data problem—it’s an insight problem. Many health systems operate in a paradox of “capacity without clarity,” lacking the visibility needed to answer basic but essential questions:
- Where is demand outpacing supply?
- Which providers have unused capacity?
- Are provider schedules aligned with their clinical FTE (cFTE) expectations?
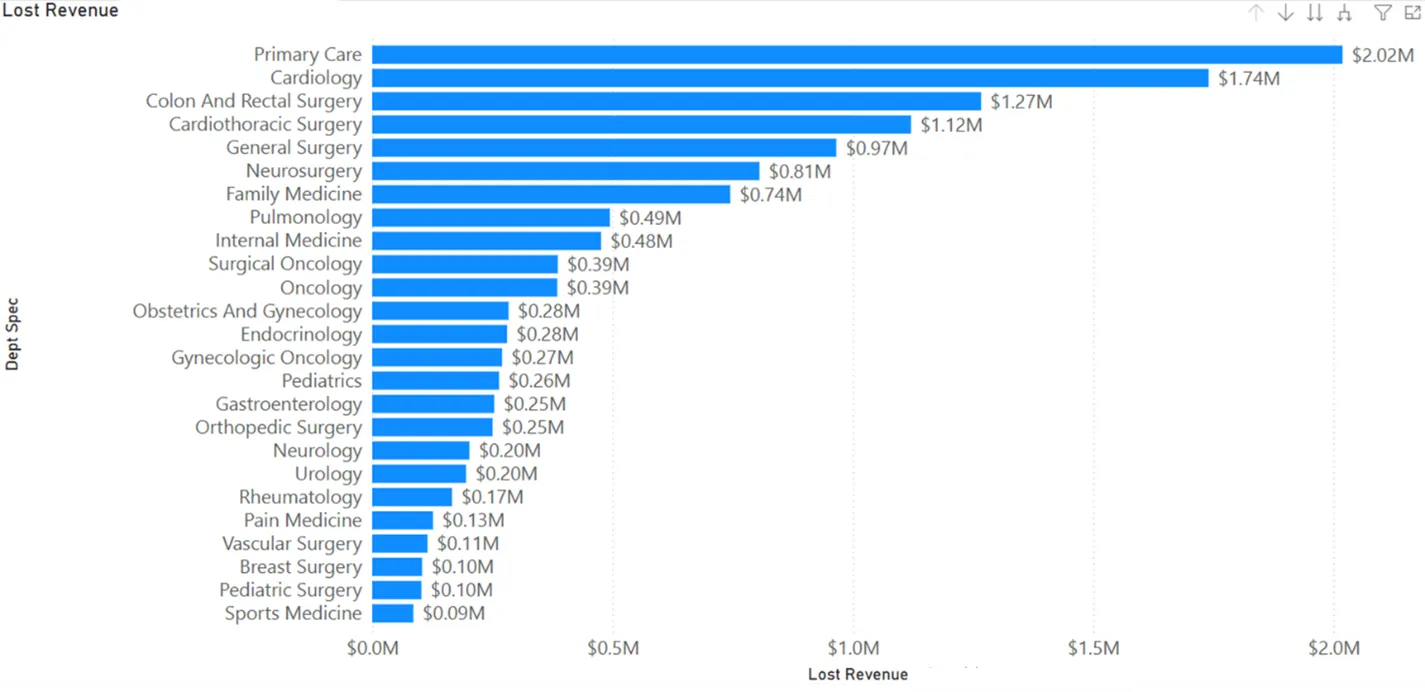
- What’s the true ROI of fixing inefficiencies in scheduling?
Schedulers often work around broken processes or restrictive templates. And EMR-generated reports don’t connect the dots between provider availability, patient demand, and throughput. Leaders are flying blind when it comes to their access vulnerabilities.
A Smarter Approach to Patient Access
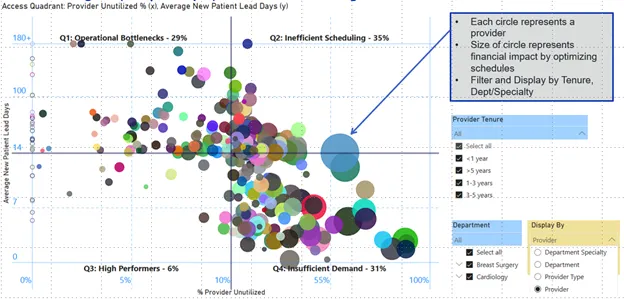
To bring clarity to this complexity, we developed Visit Boost Navigator (VBN)—a proprietary analytics tool that maps access performance across providers, practices, or service lines. VBN uses a quadrant-based diagnostic to categorize performance and surface root causes. Leaders gain actionable insights to improve scheduling, provider utilization, and patient throughput.
The Appointment Access Quadrant Framework
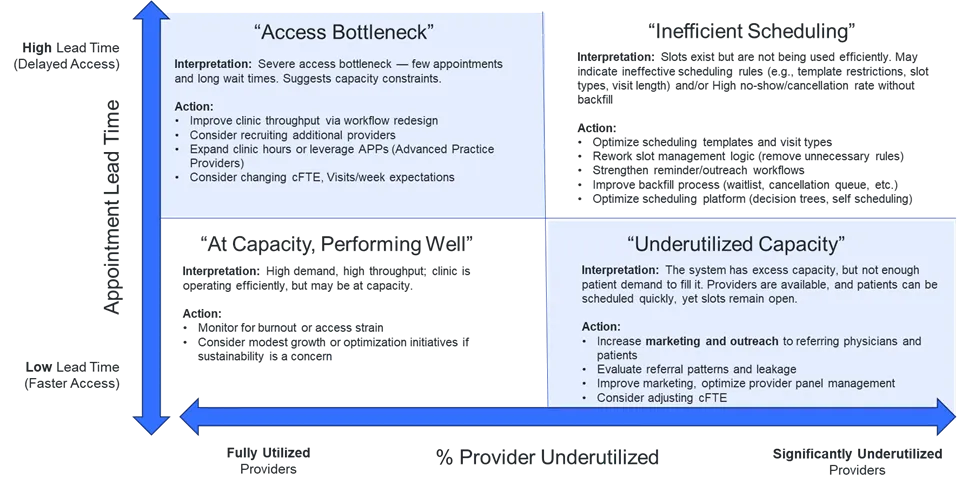
This visual model identifies four common performance zones.
1. Access Bottleneck
Quick takeaway: Long wait times despite full schedules often indicate mismatched demand and capacity or hidden inefficiencies.
Patients wait weeks or months for care, and appointment slots are consistently full. This often reflects a disparity between demand and capacity. Providers or locations in this category may be “bursting at the seams,” leading organizations to consider expanding their provider base. However, deeper analysis often uncovers more subtle causes.
In our experience, throughput and schedule misalignment are the true culprits more often than a lack of providers.
Some providers may see far more patients than others in similar roles or locations, even when their schedules are equally “full.” This variation can stem from how efficiently they use support staff or technology, meaning access issues could be solved by optimizing internal processes before investing in recruitment.
As physician enterprises grow in complexity, it’s also common to lose clarity around expected clinical time. Without a standardized definition of full-time provider cFTEs, organizations may misjudge capacity. Comparing actual schedules to expectations can reveal hidden availability and improve consistency across regions or specialties.
Key interventions:
- Audit provider schedules against cFTE expectations
- Adjust clinical days or visit targets
- Rebalance administrative vs. patient-facing time
- Leverage team-based care
- Expand provider base only after other fixes
2. Inefficient Scheduling
Quick takeaway: Appointments are available, but the system isn’t using them effectively.
In this quadrant, lead times remain long despite many open slots. This typically stems from rigid scheduling templates, mismatched slot types, or underdeveloped backfill processes. Though EMRs support complex rulesets, excessive complexity can backfire, especially when unmanaged.
Practices often want to retain control over their own schedules, which leads to variability in templates, slot types, and exceptions. While this may work at the local level, it undermines efficiency and scalability across the system. Schedule templates filled with unavailable “holds” or unique rules for each appointment type make it difficult for schedulers or patients to match availability to need.
Every system is perfectly designed to get the results it gets. - W. Edwards Deming
In the case of inefficient scheduling, that result is wasted capacity and patient frustration.
Key interventions:
- Redesign scheduling templates for consistency
- Consolidate or simplify visit types
- Strengthen cancellation and waitlist workflows
- Improve digital scheduling ability
- Train schedulers in slot utilization strategies
3. Underutilized Capacity
Quick takeaway: Low demand or referral friction is keeping available appointments empty.
Here, lead times are short and many appointment slots remain unused. In some cases, this reflects a group of newly hired providers ramping up. But when seasoned providers fall into this category, referral workflows, patient access, or demand generation may be the issue.
Referral orders may be delayed in work queues or caught in manual processes. Patients may struggle to find these providers through digital scheduling tools. In other cases, weak marketing or a lack of awareness in the community can limit new patient inflow. If these efforts are exhausted, organizations may need to redeploy providers to areas of greater need.
Key interventions:
- Evaluate and reduce referral leakage
- Streamline handoffs and referral processes
- Expand community outreach or marketing
- Improve visibility in online scheduling platforms
- Consider reassigning providers based on service line demand
4. At Capacity and Performing Well
Quick takeaway: This is the sweet spot—short wait times, full schedules, and steady throughput.
Providers in this quadrant demonstrate balance between supply and demand. Appointment lead times are short, fill rates are high, and no-shows or cancellations are minimal. Templates are well designed, and providers are consistently meeting or exceeding expected visit volumes. These teams are doing it right—but sustaining this level of performance takes attention.
Strong performance today doesn’t eliminate the need for support, recognition, or strategic foresight.
If ignored, high-performing providers can burn out, and high-functioning systems can unravel. Leaders should invest in sustaining infrastructure and seek opportunities to replicate successful practices across the organization.
Key interventions:
- Monitor for provider burnout and workload balance
- Support with infrastructure and short-term staffing pools;
- Recognize and reward success
- Use data to identify and replicate best practices
From Reactive Fixes to Strategic Access
Access challenges often don’t stem from a lack of resources, effort, data, or tools. They stem from a lack of clarity. The quadrant framework distills complex operational data into a practical view that helps organizations identify root causes and act with precision.
As access remains a top priority for executives in 2025 and beyond, health systems must move from reactive fixes to scalable, repeatable strategies.
Visit Boost Navigator equips leaders with the insights they need to shift access from a vulnerability to a strategic advantage.
Ready to Improve Access at Scale?
Let’s take the guesswork out of access improvement. Our team can help you uncover hidden capacity, realign scheduling workflows, and build sustainable access strategies.

