Clearing the Air on Professional Services Agreements (PSAs)
Discover the truth behind PSAs and how they offer alignment without sacrificing independence.
Editor’s Note: This post has been updated to reflect the current state of PSA models and address evolving trends in hospital-physician alignment.
Professional services agreements (PSAs) continue to be one of our most frequently discussed alignment models among hospitals and physician practices. These arrangements offer a flexible alternative to employment, allowing organizations to partner while preserving physician independence. At Coker, we often refer to PSAs as "employment lite" because they offer many employment benefits without fully merging entities.
PSAs have steadily evolved into a mainstream alignment strategy, with more practices and hospitals embracing their flexibility and adaptability. Yet, we continue to encounter confusion and lingering misconceptions. This post aims to clarify those misunderstandings and compare the two most common PSA structures: the Traditional PSA and the Global Payment PSA (GPPSA).
What Do Physicians Worry About?
Physicians' most common concern about PSAs is that they are a stepping stone to full employment. That perception is understandable, particularly with the Traditional PSA, which often does evolve into employment. However, it’s essential to recognize that PSAs can preserve autonomy and provide long-term alignment without employment, especially under the GPPSA model.
Comparing the Two PSA Models
Both Traditional and Global Payment PSAs offer alignment without full acquisition. Here's how they differ:
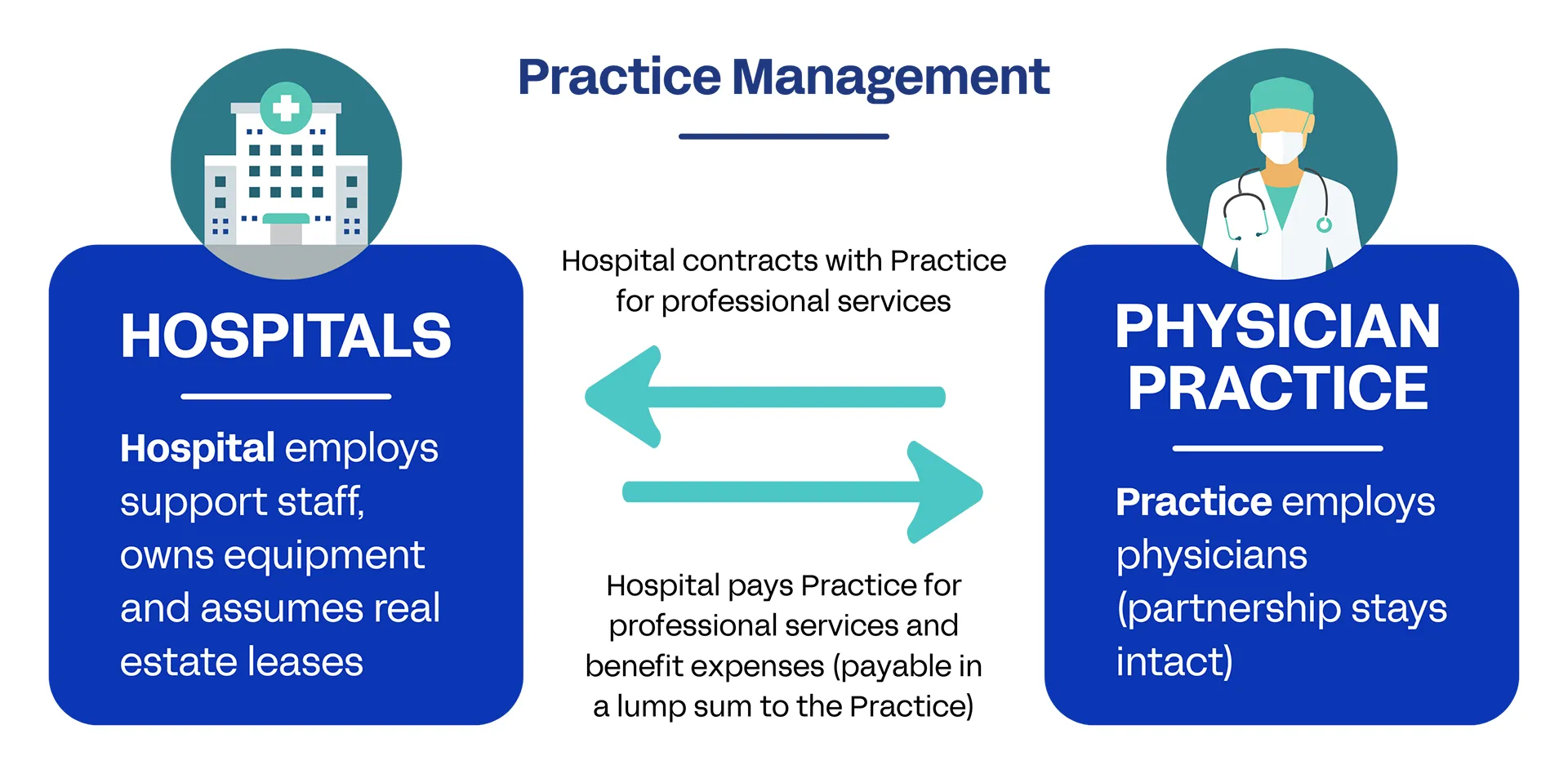
Practice Management
The hospital or partnering entity assumes responsibility for practice management. The physicians remain employed by the original practice, which stays legally intact. They contract with the hospital or other partnering entity for professional services. Advanced practice providers may or may not remain within the practice structure.
Payment
The hospital controls payer contracts and handles billing for all professional charges. Physicians are compensated based on productivity (typically wRVUs), and the practice continues to provide benefits, funded through its total economic package.
This model closely mirrors employment—but without formally employing the physicians.
When It Makes Sense
Traditional PSAs are ideal as a trial run for practices considering full employment. They also help practices burdened by administrative responsibilities or seeking to improve payer rates by leveraging hospital contracts.
Global Payment PSA (GPPSA)
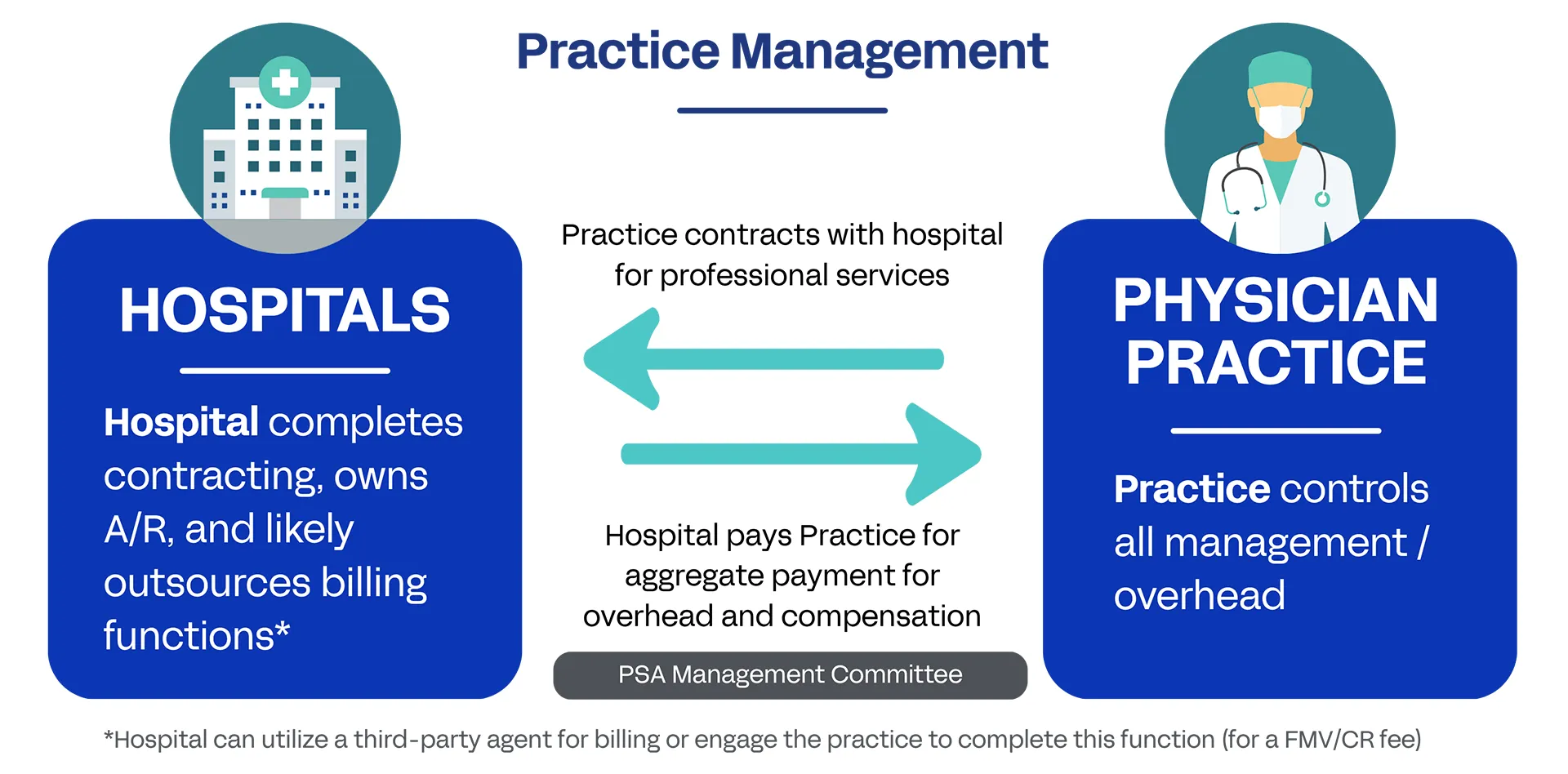
Practice Management
The practice remains fully operational and independent. The key distinction is that the hospital takes over the revenue cycle, including contract negotiations, billing, and collections.
Payment
Physicians are paid based on productivity (usually wRVUs) and may also earn incentive-based compensation. Overhead is reimbursed on a fixed or budgeted basis, with occasional variable reimbursement per wRVU.
GPPSAs emphasize autonomy and operational continuity while offloading revenue cycle burdens.
When It Makes Sense
GPPSAs are best suited for groups that want to maintain independence, reduce administrative pressure, and gain access to better payer contracts without adopting an employment-like structure. With a solid foundation of trust, these arrangements can last for years without transitioning to full employment.
Clearing Up the Confusion
The belief that PSAs inevitably lead to employment is a myth. Practices have a spectrum of options for partnering with hospitals or health systems while retaining the level of autonomy they desire. Whether seeking full alignment or a light-touch arrangement, the PSA model can be customized to meet both parties' strategic and operational needs.
This is often where we step in. Coker consultants help assess each party's goals, evaluate fit, and design PSA structures that foster alignment while minimizing disruption.
What to Do Next
📘 Read our white paper on PSA models for deeper insight into Traditional and Global Payment PSAs
💼 Explore our strategic alignment services to see how we help organizations structure sustainable partnerships
📅 Talk to a Coker consultant about designing the right PSA model for your organization

.webp)
